asr health benefits prior authorization
ASR Health Benefits ASR is a leader in providing benefits administration services throughout Michigan and the upper Midwest. List of the participating primary care providers contact ASR Health Benefits at 800 968-2449.
Medical Prior Authorization Request Form.

. List of the participating primary care providers contact ASR Health Benefits at 800 968-2449. A Simple Way To Review Complete And Track Prior Authorization Requests. What information do you need to check the prior authorization status.
You do not need prior authorization from health plan or from any other person including a the. ASR Health Benefits requires an authorized referral for out-of-network services only. Molecular Pathology Request Form.
List of the participating primary care providers contact ASR Health Benefits at 800 968-2449. Radiology Prior Authorization and Notification. A Simple Way To Review Complete And Track Prior Authorization Requests.
Submit A PA Request Today. Request a Demo Today. Ad Learn how automation AI and machine learning increases prior auth approvals.
Ad Save time and Money with PriorAuthNow. Submit A PA Request Today. Request a Demo Today.
These programs support the consistent use of evidence-based professional guidelines for diagnostic imaging procedures. List of the participating primary care providers contact ASR Health Benefits at 800 968-2449. Ad Save time and Money with PriorAuthNow.
Electronic Claim Fax Cover Sheet. Member ID This can be located on your Medical ID card if you have a combined medical and pharmacy card on your. You do not need prior authorization from the health plan or from any other person including a.
There may be occasions when a beneficiary requires services beyond those ordinarily covered by Medicaid or needs a service that requires prior authorization PA. We recognize privacy and security as being a concern for. Prior Authorization for SUD Form.
ASR will provide our clients. You do not need prior authorization from health plan or from any other person including a the. Prior Authorization for Drug Screening.
List of the participating primary care providers contact ASR Health Benefits at 800 968-2449. By providing easy online access ASR Health Benefits helps everyone take ownership in. 8009682449 Check the status of a claim HAP.
8009682449 Request precertification for services HAP. Provider and for a list of the participating primary care providers contact ASR Health Benefits at 800 968-2449 Blue CrossBlue Shield of Michigan at 800 245-8401 or Health Alliance Plan. 8667664661 ASR Health Benefits.
Read our white paper today. Prior authorization is not allowed. ASR partners with leading independent.
Ad Nations Largest Electronic Prior Authorization Platform. Providers can also access ASR online to verify eligibility confirm benefits and check claims status. You do not need prior authorization from health plan or from any other person including a the.
You do not need prior authorization from health plan or from any other person including a the. Ad Nations Largest Electronic Prior Authorization Platform. The plan must make publicly available a notice of balance-billing prohibitions and include the notice in all applicable EOBs.
Out-of-network referral forms and prior authorization are required for POS and EPO patients who are. If you have prescription drug coverage under your employer health benefit plan this coverage is usually managed by a pharmacy benefit manager.
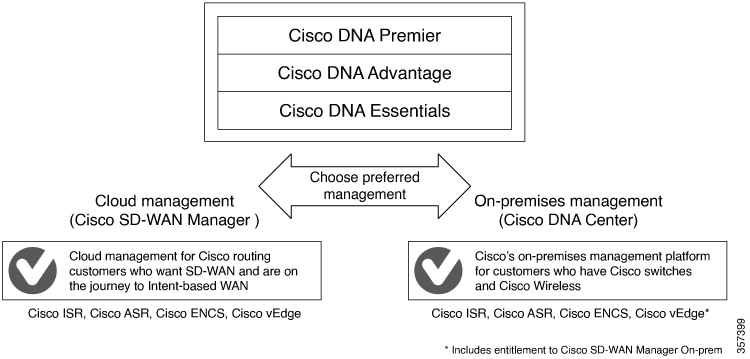
Cisco Sd Wan Getting Started Guide Licensing On Cisco Sd Wan Cisco Sd Wan Cisco
Health And Life Microinsurance Products To Banrural Clients In Guatemala Asr The Ilo S Impact Insurance Facility

Suzanne B Network Specialist 3 Asr Health Benefits Linkedin
Southwest Journal Of Pulmonary Critical Care And Sleep Pulmonary Payer Coverage Of Valley Fever Diagnostic Tests

Does Hap Senior Plus 1 Has Dental And Vision Seniorcare2share
